On the occasion of Liver Cancer Awareness Month, the European Parliament ‘Challenge Cancer’ Intergroup hosted the virtual event ‘Opportunities for Hepatitis Related Cancer Prevention in Europe’s Beating Cancer Plan’. The webinar, which took place on 28th October, discussed how the implementation of Europe’s Beating Cancer Plan can make a significant contribution to reducing hepatitis-related liver cancer.
Europe’s Beating Cancer Plan has rightly recognised hepatitis B vaccination and hepatitis C treatment in the context of cancer prevention. Unfortunately, the awareness of viral hepatitis B and C as preventable cancer risk factors is not always well understood. This is true for the general public, specific risk groups, and even amongst healthcare professionals. The event was organized with the support of the European Cancer Patient Coalition (ECPC), the Association Collaborating on Hepatitis to Immunize and Eliminate the Viruses in Europe (ACHIEVE) and the European Association for the Study of the Liver (EASL).
MEP Aldo Patriciello, Co-Chair of the Challenge Cancer Intergroup and BECA member, highlighted in his opening remarks: “Scientists from the International Agency for Research on Cancer have pointed out that tackling viral hepatitis B and C is essential to significantly prevent cancer and reduce its burden, which is significant also for European countries. My amendments to the draft BECA report ‘Strengthening Europe’s report in the fight against cancer’ thus aim to ensure that we make full use of the tools available in Europe’s Beating Cancer Plan to prevent hepatitis-related liver cancer, including adding liver cancer to the list of recommended screening programmes.”

To better prevent hepatitis-related liver cancer, Professor Romana Jerković MEP, BECA member, highlighted the importance of the Council Recommendation on vaccine preventable cancers, as well as means to improve people’s health literacy, such as the EU Mobile App for Cancer Prevention and an updated European Code Against Cancer. MEP Jerković also highlighted the need for Member States to work more closely together: “There are huge inequalities across Member States. One of the future goals will be European Health Union. Although Member States are responsible for health, we have had lots of problems in common so we can be successful in beating cancer and other diseases if we are united and share good practices.”
MEP Radan Kanev, Member of the ENVI Committee, stated: “We must make sure that the elimination of viral hepatitis B and C through greater awareness of transmission risks, vaccination against hepatitis B for all children and adult risk groups, a much higher diagnosis rate and linkage to care and cure for hepatitis B and C, will be embedded in both the Europea and also national cancer plans as effective means to prevent cancer. We must not forget, that the vast number of people infected with viral hepatitis B and C, many of whom are part of vulnerable populations, are still undiagnosed. Finally, we need better monitoring throughout Europe, so we are no longer flying blind. The ECDC mandate extension, which is currently under discussion in Trilogue, can make a significant contribution in this regard and support Member States.“

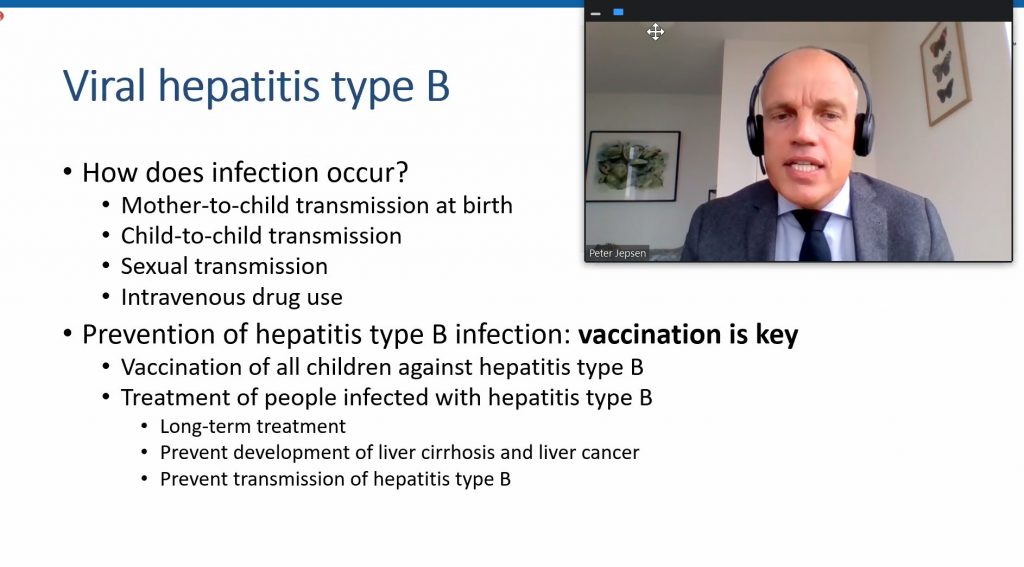
Professor Peter Jepsen, Policy and Public Health Committee EASL, highlighted that over the past two decades, there has been a 70% increase in liver cancer-related mortality in the region and the fact that Viral hepatitis types B and C cause liver cirrhosis and liver cancer. 80-90% of patients with liver cancer have an underlying chronic liver disease: liver cirrhosis which a is a steppingstone towards liver cancer. He called on policymakers to catch “2 birds with 1 stone: eliminate viral hepatitis types B and C and thus eliminate risk factors for liver cirrhosis and liver cancer”.
Professor Maria Buti, EU Policy Councillor and member of the governing board of the European Association for the Study of the Liver (EASL) highlighted: “Chronic HBV and HCV infections are often asymptomatic until later stage. 2/3 of adults with HBV and 1/3 with HCV are unaware of their condition. To eliminate/control hepatitis viruses by 2030, we must improve prevention, screening, and linkage to care targets”. Prof. Maria Buti told the available tools and instruments to achieve these goals and at the same time reduce the risk of liver cancer by implementing prevention programmes for HBV through vaccination and treatment and for HCV through screening and treatment as prevention.
ACHIEVE (Associations Collaborating on Hepatitis to Immunize and Eliminate the Viruses in Europe), Co-Chair and former Hepatitis C patient George Kalamitsis stated: “We must share information about the transmission risks for viral hepatitis B and C, about testing and treatment options, when informing people onhowtolowertheircancerrisk. Initscurrentform,theEuropeanCodeagainstCancerfailstodothis.This is why we need to update the European Code Against Cancer urgently.”
About Hepatitis and Liver Cancer – Europe’s deadliest preventable cancer
Viral hepatitis B and C, recognised by WHO as cancer-preventable risk factors, are responsible for up to 76% of all liver cancer cases worldwide.1 Hepatitis B is preventable with a safe and effective vaccine available, as well as treatments to manage the infection. Hepatitis C is curable. In the European Union, around 10 million people live with chronic hepatitis B and C and a majority are undiagnosed.2 Every year up to 90,000 people with chronic viral hepatitis develop liver cancer.3 Liver cancer has the lowest survival rate among all cancers monitored by the European Commission,4 making it the deadliest preventable cancer in the EU. Modelling suggests that cancer prevention efforts targeting viral hepatitis C could reduce liver cancer incidence by 70% and liver-related death by 65%,5 especially among high-risk groups who are associated with higher incidence rates.6 As highlighted by researchers from IARC, greater efforts to tackle important infections, namely viral hepatitis B and C, could make a significant contribution to prevent cancer and reduce the cancer burden.7
Hepatitis Elimination by 2030 – The need for urgent action
In 2016, EU countries committed to combat and end hepatitis as a public health threat by 2030, in line with the WHO targets and the UN SDGs. Five years later, it is increasingly clear that the target will not be met unless countries urgently address the massive gaps in vaccination, treatment, diagnosis and linkage to care and data generation. Whilst COVID-related disruptions have worsened the situation and reversed progress, the pandemic has also shown how much countries can achieve in communicable disease control in a short time span.
References
De Martel C, Georges D, Bray F, Ferlay J, Cliffor GM (2020). Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis. The Lancet: Global Health, 8(2).
ECDC (2019). Systematic review on Hepatitis B and C prevalence in the EU/EEA, p. 2. Available at https://www.ecdc.europa.eu/en/publications-data/monitoring-responses-hepatitis-b-and-c-epidemics-eueea-member-states-2019
European Cancer Organisation. (2020) It Can Be Done – Beating Inequalities in Cancer Care. Action Report. Accessed from http://www.europeancancer.org/resources/164:beating-inequalities-in-cancer-care.html
European Union HCV Collaborators. (2017). Hepatitis C virus prevalence and level of intervention required to achieve WHO targets for elimination in the European Union by 2030: a modelling study. Lancet Gastroenterol Hepatol, 2(5), pp. 325-336.
International Agency for Research on Cancer (WHO) (2020). Liver Cancer Factsheet. Accessed from https://gco.iarc.fr/today/data/%20factsheets/cancers/11-Liver-fact-sheet.pdf
Joint Research Centre (European Commission). European Cancer Information System – ECIS. Estimates of cancer incidence and mortalility in 2020, for all cancer sites. Accessed from https://ecis.jrc.ec.europa.eu/explorer.php?$0-0$1-AE27$2-All$4-1,2$3-Al-%20l$6-0,85$5-2008,2008$7-7,8$CEstByCancer$X0_8-3$CEstRelativeCanc$X1_8-3$X1_9-AE27$CEstBySexByCancer$X2_8-3$X2_-1-
Wild, C. P. (WHO) (2020). World Cancer Report: Cancer Research for Cancer Prevention, p. 61.
